HIV is one of the most prevalent diseases in the world, and like cancer and other rare diseases, it has no cure.1 Each year, the rising number of HIV cases becomes an increasing concern, but doctors and scientists are continuously researching to find a cure.
According to WHO data, 85.6 million people had contracted HIV and 40.4 million people had died from the disease by 2020. Despite these alarming numbers, many people are still unaware of HIV infection and related safety measures.
Getting rid of HIV is a complex issue that cannot be solved overnight. Even if the disease itself were miraculously cured, the stigma and taboo surrounding HIV would still take years to normalize. However, as citizens of the 21st century, we have a responsibility to end the stigma around HIV and educate ourselves and future generations about the importance of HIV awareness. Doing so will not only allow us to live more harmonious and peaceful lives, but it will also end the discrimination against people living with HIV.
Although PrEP medication has been around for some time, its mainstream use is still rare. This is likely due to the stringent safety regulations surrounding HIV medication. However, PrEP is now being popularly recognized and utilized by both individuals living with HIV and their sexual partners.
In this blog, we’ll learn all about HIV and how PrEP can assist in HIV safety!
Firstly, let’s start with understanding HIV.
What Is HIV?
Human immunodeficiency virus/ HIV (as the name suggests) is known to cause an infection that targets the body’s immune system. If HIV persists for a long time in a human then it can potentially cause AIDS- autoimmune deficiency syndrome. Since HIV attacks white blood cells and weakens immunity, its presence often leads to the development of life-threatening diseases like tuberculosis, infections, and even cancers.
As discussed earlier, if someone contracts HIV they have to live with it throughout their life. However, with relevant medical care, symptom management, etc., patients can often lead a healthy and content life.
Now that you know about HIV, let’s discuss its history.
History Of HIV
HIV originated from a specific breed of Chimpanzees living in Central Africa. Studies show that HIV may have reached humans from Chimpanzees as far back as the 1800s, but the first case of AIDS (acquired immunodeficiency syndrome) was recognized in the United States in 1981. At the time, it was observed that many young homosexual men were getting infections frequently and developing cancers.
The kind of virus similar to HIV that attacks Chimpanzees is called the simian immunodeficiency virus.
It is believed that HIV was transmitted to humans when a group of people hunted Chimpanzees for meat and came into contact with their infected blood. HIV may have originated in Africa, but it has unfortunately spread to all parts of the world.
AIDS has existed in the United States from the mid-late 1970s.
Symptoms Of HIV
Did you know that there are three stages of HIV, and each stage has its own set of symptoms? We’ll discuss all the stages and symptoms in detail, but first, let’s talk about the common symptoms.
Most people who are infected with HIV experience flu-like symptoms within the first two to four weeks of exposure. These symptoms may include:
- Chills
- Fatigue
- Fever
- Inflamed lymph node(s)
- Mouth ulcers
- Muscle aches
- Sore throat
- Rashes
However, it is important to note that not all flu-like symptoms are a sign of HIV infection. It is also possible for an individual to have no HIV symptoms at all. This is why individuals need to take proactive testing.
After learning a little about HIV’s symptoms, let’s now take a look at its different stages.
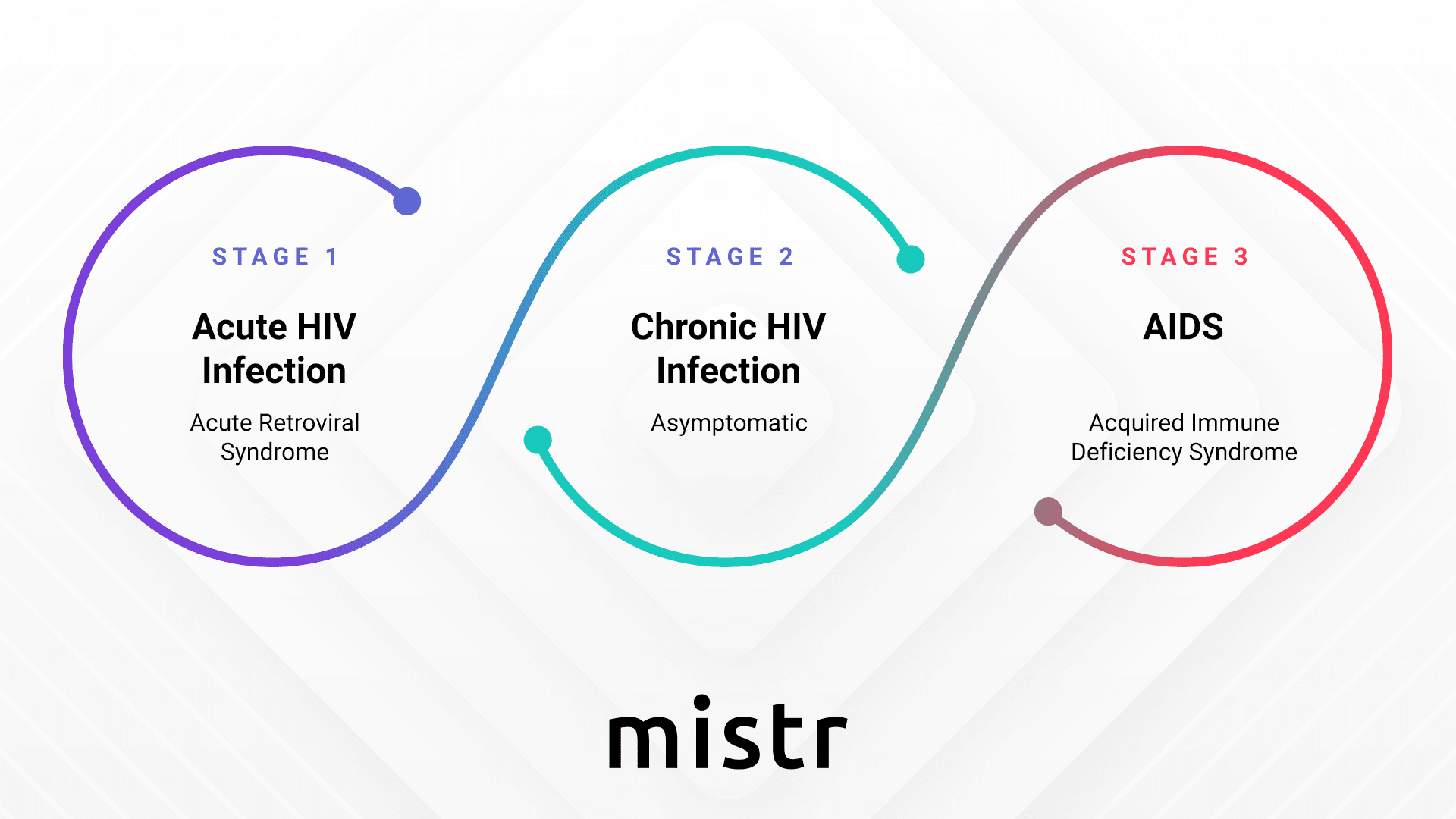
Different Stages Of HIV
Individuals with HIV infection, who do not get medical attention in time can experience progressed stages of the disease. However, thanks to medical advancements, progression to the last, or thoracic stage of HIV has become less common than it was in the early years of the HIV epidemic.
Let’s briefly discuss each stage of the HIV infection.
Stage 1: Acute HIV Infection
- During this stage, the infected individual has a higher amount of virus in their blood.
- They may also experience flu-like symptoms.
Stage 2: Chronic HIV Infection
- In this stage, the symptoms become dormant, although the virus remains active and continuously reproduces inside the body.
- This phase is often referred to as asymptomatic HIV infection or clinical latency due to the inactive nature of HIV’s symptoms (during this stage).
- If an infected person does not receive medical treatment during this stage, the infection may last longer, or diseases progress to the next stage sooner.
Stage 3: Acquired Immunodeficiency Syndrome (AIDS)
- It is the final stage of HIV infection.
- If a person reaches this stage, they potentially have a high viral load, meaning they can easily transmit the HIV infection to others.
- Individuals with AIDS have a highly compromised immune system, making them more susceptible to infections.
- Lastly, if a patient with AIDS does not receive any form of treatment (for HIV), their life expectancy drops as low as 3 years.
HIV Transmission
Many people know that HIV is transmitted through the exchange of bodily fluids, such as breastmilk, blood, semen, and vaginal secretions. It can also be transmitted from mother to child during pregnancy.
But what about other forms of contact, like kissing, shaking hands, sharing food, or hugging? Can HIV be transmitted through these activities?
The answer is NO! HIV cannot be transmitted through casual contact. You cannot get HIV from sitting next to someone with HIV, touching their skin, or sharing food or drinks with them.
This is because HIV is a fragile virus that cannot live outside the body for very long. It also cannot penetrate the skin unless there is an open wound or sore.
So, while it’s important to be aware of how HIV is transmitted and take steps to protect yourself, you can rest assured that you won’t get HIV from simply being around someone with the virus.
HIV Testing: What You Need To Know?

There are now a variety of tests available to detect HIV, including blood tests, saliva tests, and rapid self-tests. The most common HIV tests are:
- Antibody/Antigen Test
This test looks for HIV antibodies and antigens in the blood. Antibodies are proteins that the body produces to fight infection, and antigens are substances found on the surface of HIV. Antibody/antigen tests can detect HIV after a few weeks of exposure.
- Antibody Test
This test looks for HIV antibodies in the blood or saliva. Antibody tests are the most common type of HIV test and can be done at home or at a doctor’s office. Antibody tests can detect HIV within three to twelve weeks of exposure.
- Nucleic Acid Test (NAT)
This test looks for HIV RNA in the blood. RNA is the genetic material of HIV. NATs are the most sensitive HIV tests available.
Advanced HIV Testing
In the previous section, we discussed the tests that are required during the initial exposure to HIV. However, in cases where HIV has progressed, the same set of tests may not be helpful. That’s why doctors have also developed different tests and parameters.
Here are some additional tests that help doctors learn about the type of HIV a patient may have. This information further helps them to develop a proper treatment course:
- CD4 count test: This test measures the number of CD4 cells in the blood. CD4 cells are a type of white blood cell that helps fight infection. HIV destroys CD4 cells, so a low CD4 count can indicate a weakened immune system and a more advanced stage of HIV infection.
- Viral load test: This test measures the amount of HIV in the blood. A high viral load can indicate that the virus is replicating rapidly and that the infection is progressing.
- Resistance test: This test checks to see if HIV is resistant to certain drugs. Antiretroviral drugs are used to treat HIV and slow the progression of the disease. A resistance test can help doctors determine which drugs are most likely to be effective for a particular patient.
Additional Health-Related Tests For People With HIV
When people are living with HIV, they are more likely to develop certain infections and health complications. To monitor for these conditions, doctors may recommend a variety of lab tests, including:
- Anal cancer: This test looks for precancerous cells or cancer cells in the anus. Anal cancer is more common in people with HIV because HIV weakens the immune system.
- Cervical cancer: This test looks for precancerous cells or cancer cells in the cervix. Cervical cancer is also more common in people with HIV.
- Cytomegalovirus (CMV): This test looks for CMV infection. CMV is a common virus that can cause serious illness in people with HIV.
- Hepatitis B and C: These tests look for infection with hepatitis B or C viruses. Hepatitis B and C can cause serious liver damage, especially in people with HIV.
- Kidney damage: This test looks for signs of kidney damage. Kidney damage is more common in people with HIV because HIV can damage the kidneys.
- Liver damage: This test looks for signs of liver damage. Liver damage is more common in people with HIV because HIV can damage the liver.
- Toxoplasmosis: This test looks for toxoplasmosis infection. Toxoplasmosis is a common parasite that can cause serious illness in people with HIV.
- Tuberculosis (TB): This test looks for TB infection. TB is a serious bacterial infection that can be fatal in people with HIV.
These tests are important for people with HIV because they can help doctors detect infections and health complications early when they are most treatable. Early treatment can help prevent serious illness and death.
In addition to the tests listed above, people with HIV may also need to have other tests done, depending on their individual risk factors and health needs.
HIV Treatment: Role Of PrEP
So even though HIV has no cure, it still has treatment options. Yes, you heard it right! Medical science might’ve not found the cure for HIV but…it can be prevented- with the help of PrEP.
PrEP decreases the risk of contracting HIV by 99%! How does it do that? Well, to know that keep on reading!
What Is PrEP?
PrEP stands for pre-exposure prophylaxis. It is a drug that decreases an individual’s risk of contracting HIV either from unprotected sex or injectables.
How Does PrEP work?
PrEP works by preventing the further growth of HIV inside the body.
How To Take PrEP?
An individual can take PrEP in two ways:
i. One pill every day for the next seven days, for as long as it’s required before coming in contact with HIV infection.
ii. On-demand before having unprotected sexual intercourse.
Who Should Consider Taking PrEP?
Anyone who is sexually active or often engages in high-risk activities must consider taking PrEP. Though, there are some cases, that make taking PrEP imperative for certain individuals. Let’s discuss each of these cases thoroughly!
Case 1: Test Negative For Hiv Infection But Have A High Risk Of Contracting HIV
Sexually active individuals, who have multiple sexual partners, or engage in high-risk sexual behaviors should seriously consider PrEP. As it’s known to substantially reduce the probability of contracting HIV infection. That as a result may help individuals maintain a healthy sex life.
Case 2: Identity As Gay Or Bisexual
The gay and bisexual communities are notably impacted by HIV, as they often engage in unprotected anal sex. If an individual belongs to this group, taking PrEP should be a priority to ensure optimal sexual health.
Case 3: Have an HIV-Positive Partner
While we strongly advocate for caution in engaging in sexual activities with an HIV-positive individual, we understand that love knows no boundaries. If an individual has a partner, who is HIV-positive but still wishes to be intimate with them, then they should consider taking PrEP.
Case 4: Engage In Risky Sexual Behavior Regardless Of Sexual Orientation
PrEP significantly reduces the risk of HIV transmission by up to 99%. Whether a person identifies as gay or straight, taking PrEP facilitates practicing safe sex, minimizing the chances of contracting an HIV infection.
Case 5: Recently Had Or Have A History Of Stds
Individuals with a recent history of STDs face an increased risk of contracting HIV. However, if they take PrEP, their chances of contracting HIV in the recovery phase are lower, helping the individual to live a healthy sex life.
Case 6: Engage in Sexual Intercourse With Individuals Whose Sexual/HIV History Is Unknown
While unprotected sex is discouraged, unforeseen circumstances may arise. Individuals who often engage in impromptu sex with strangers must consider/ be taking PrEP.
Case 7: Frequently Share Injectables Or Drugs
Substance abuse is never advisable. However, if an individual has a history of drug use or frequently does drug abuse. Then considering PrEP medications can significantly reduce their risk of contracting HIV infection.
Until now, you have gained a considerable amount of knowledge on PrEP. And we’re sure that some of you may even have started thinking about taking it! However, before you make the final choice, we want y’all to take a look at the brief discussion on PeEP’s effectiveness and limitations.
Effectiveness Of PrEP
With taking PrEP one must remember that: Consistency is the key!
If a man plans to have anal sex with an HIV-positive person or is simply soon to exchange in any other high-risk activity then they should have PrEP from 7 days prior. Though, if a woman wants to attain full protection from PrEP (for participating in vaginal sex with an HIV-positive individual) then she should start taking it 21 days before.
In the following, we have mentioned some of PrEP’s other benefits:
- Highly effective when taken as directed: PrEP is very good at preventing HIV infection when it is taken exactly as prescribed by a doctor.
- May decrease anxiety regarding HIV acquisition: PrEP can help people who are worried about getting HIV to feel more relaxed and in control of their sexual health.
- Minimal adverse effects, most of which resolve in a brief time or can be managed: PrEP has very few side effects, and most of them are mild and go away on their own. However, if someone experiences side effects for a long, then they should consult their doctor.
- Good safety profiles in people who do not have HIV: PrEP is safe to consume for people who do not have HIV. However, some people may still experience side effects such as nausea, vomiting, diarrhea, headache, and fatigue, but these side effects are usually mild.
Limitations Of PrEP:
- Protection correlates with adherence to the dosing schedule: PrEP is more effective at preventing HIV infection when it is taken exactly as prescribed by a doctor.
- No significant protection against STIs other than HIV: PrEP is effective against HIV but does not protect against other sexually transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis.
- Limited to no data for pregnant women: PrEP is great but it hasn’t been tested thoroughly on pregnant or breastfeeding women. Therefore, their use is limited to only men and non-pregnant and non-nursing women.
Till now we have extensively talked about HIV and PrEP. Now the only question remains- from where can you get PrEP? Well to find the answer to that just have a peek at the next section.
Explore HIV Safety With Hey Mistr’s PrEP!
We at Hey Mistr get it – sex is important! But we also realize that taking care of one’s health for a long and fulfilling life is also crucial. And there come times when a person’s health may get compromised due to some decision they need to make in life.
To safeguard a person’s sexual choice and health, Hey Mister introduces PrEP. It’s something that may help individuals wanting to be intimate with their partners who have HIV or who often engage in high HIV-risk activities. Either case, we at Hey Mister do not judge, but rather respect your decision and focus on working day in, and day out to provide you with the best HIV safety medications.
Are you interested in knowing how it’s done? First, take a glance at the upcoming section!
Hey Mistr- One Stop Solution For Your HIV Safety Needs!
We like to go the extra mile, be it in bringing you the best medication for HIV prevention or taking your sign-up! At Hey Mistr, every little detail matters.
So, whenever you sign up for our PrEP plan, you’ll have to complete 6 phases. Performing these phases helps us get to know you better and get you the medications as soon as possible!
Phase 1: Health Assessment Before Commencing PrEP
Our dedicated team will conduct a comprehensive health assessment. They will ask you a series of questions about your health to tailor their PrEP recommendations to your specific needs.
Phase 2: At-Home Testing to Ensure You Are HIV-Free
Once your assessment is taken and shared with our healthcare experts, you will receive a complimentary at-home test. This painless test can be done by you and would require a few minutes. After we get your samples, our experts will analyze them and provide you with your HIV status results.
Phase 3: Physician Consultation Once the Test Results Are Ready
A licensed doctor will carefully review your test results and then based on these results, they will prescribe the appropriate medication. Throughout this process, our expert medical team will be available to assist you. So that if you get any last-minute doubts they can help in guiding you.
Phase 4: Convenient Home Delivery
Once everything gets a “go-ahead” from our medical experts your first installment of PrEP medication will be delivered straight to your doorstep at zero extra cost. So you don’t need to worry about any shipping fees.
Phase 5: Streamlined Administrative Process
Worried about whether your insurance will cover this PrEP medication or not? Don’t fret as Hey Mistr will handle all the necessary paperwork on your behalf! Our dedicated team works with your insurance company and patient assistance programs to ensure that you receive the required PrEP medication without incurring any unnecessary expenses.
Phase 6: Automated Check-Ins
We will also be sending you automated reminders every 3 months to refill your PrEP medication, ensuring you never run out of this vital supply.
Everything will be taken care of from the end, so you’d just have to worry about taking your PrEP medications on time!
Final Take
We hope that by reading this blog, you have gained a sufficient amount of insights into PrEP. Taking PrEP is a personal choice, which at times, may be dependent on financial issues or even societal factors. However, we encourage you to break the shackles of double standards and be your true self. Doing so will not only make you happier from the inside but will also keep you healthy – just as taking PrEP will do!
In the end, we’d like to thank you for reading! And if you’re considering taking PrEP, don’t forget that we’re just a “SIGN UP” away!